The oncologists have long argued, convincingly, that the ‘profit’ from chemotherapy makes up in part for the poor payment they receive for the cognitive work they do, including careful deliberation about the most serious of diagnoses, and nonbillable patient and family counseling. The financial incentive to give more chemotherapy, and to prefer brand-name (high margin) chemotherapy, has always seemed like a bad idea.
Most of us don’t ever want to need an oncologist. But if we do, we don’t want the oncologist to make much more money if she treats us with more expensive chemotherapy!
Medicare made this system dramatically more rational six years ago. CMS initially moved the price from 95% of Average Wholesale Price to 85% of AWP, and then moved to 6% above average sales price. AWP is a fiction – and almost all medications can be purchased at dramatic reductions from AWP. Estimates suggested that the markup for chemotherapy agents from Medicare decreased on average from 22% to 6%.
Health Affairs just published an evaluation of the results of Medicare’s change in payment methodology on the web. The article was briefly mentioned in yesterday’s New York Times. The researchers reviewed Medicare claims data for over 200,000 patients with the diagnosis of lung cancer.
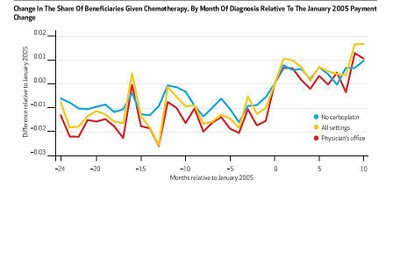
The results are stunning. In the context of these payment cuts, physicians
è Prescribed chemotherapy to more patients (18.9% got treatment within a month of diagnosis, compared to 16.5% before the payment changes
è Dramatically increased the use of one medicine, docetaxel, where price decreased by just 8% and where a high price means that the 6% margin represented a larger profit for the oncologist.
è Paclitaxel use fell, and it represented a much lower portion of all chemotherapy administered. (The authors present a graph showing a huge decline, but when I multiply out the percent of those given chemotherapy with the likelihood they got Paclitaxel, it appears that the utilization is flat while the utilization of many other drugs increased. I’ve put these calculations in this appendix) http://isites.harvard.edu/fs/docs/icb.topic659062.files/chemotherapy%20paclitaxel.xls
è Another chemotherapy drug which did not have a dramatic price cut nonetheless showed a drop in utilization
The authors note that economic theory suggests that when physicians face a fee cut that will have a large impact on their income, they increase utilization. On the other hand, when there is a fee decrease that impacts merely a small share of physician income, the affected services have lower utilization.
This is an important insight as we review how to control medical inflation. Many support a large recalibration of health care reimbursements to move income from procedural specialties to cognitive specialties -- especially primary care. However, this study suggests that very large or across-the-board fee schedule decreases would be likely to lead to much higher utilization in affected specialties.