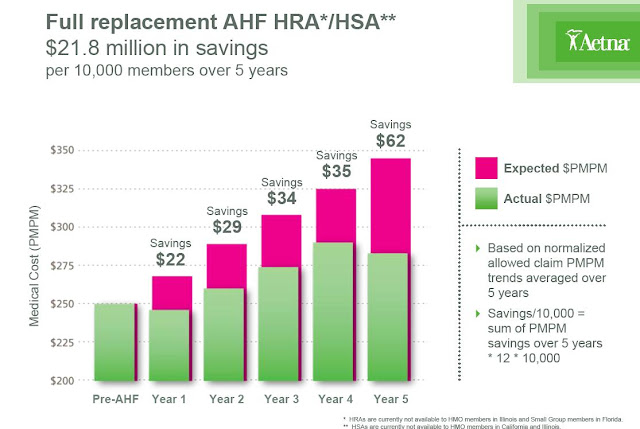
Today’s Managing Health Care Cost Indicator is $21.8 million.
Or maybe it’s 40%
 |
| Click image to enlarge. |
I’ve been reviewing two related but contradictory documents over the past day.
o Lowers costs by 11% (or $21.8 million per 10,000 members)
o These savings increase year over year
o Members
o use more primary care and preventive services but fewer nonroutine services
o Have fewer inpatient admissions
o Are more engaged
o Have fewer “gaps in care”
o Almost three quarters of members with associated health care savings accounts do not exhaust these accounts each year.
This is an upbeat document – although the underlying data has not been subject to peer review. I've only reviewed the press release and the glossy powerpoint. It’s likely that the high deductible plan had younger, healthier, lower risk members, and this alone could explain some of these findings.
 |
| Click image to enlarge. |
The Journal of General Internal Medicine e-published an evaluation of foregone care in those with chronic illnesses, surveying Massachusetts
The proof is in that HDHPs save money, and the dollar savings don’t seem to be limited to the first year or two (although there are still potential selection bias issues). It’s also clear despite the happy faces and fluorescent green graphics that members of HDHPs are less happy with their health plans, and they self-edit care. Sometimes HDHP members forego care that would have been a waste anyway –but sometimes they forego care that could help them live better quality and more productive lives.
The danger of having no health insurance at all is far greater than the danger of delayed or foregone care in a high deductible health plan. I’ll have more on that in the next day or two. Health care reform and the rising cost of health care has driven more and more employers to health plans that have high deductibles, and many of the future health insurance exchange programs are also likely to have high deductibles.
We have to work harder to lower the underlying cost of health care so that we don’t have to cost-shift as much to patients, who are at serious risk of being underinsured now. That risk will continue to increase in the near future.











