Today’s Managing Care Indicator is 37 Last May, a group of intrepid oncologists identified five behavior changes and five attitude changes that could allow oncologists to increase the value of health care, largely by not performing certain tests and not administering chemotherapy in certain circumstances. This is an important effort, encouraged by the Institute of Medicine. The American College of Physicians, the professional society of internists, has followed suit with an expert panel that identified 37 diagnostic tests that should not be provided to patients. Each of these tests does little to decrease uncertainty, and many of them are likely to lead to false positives which induce further unnecessary tests. The list is at this URL, which is unfortunately behind a paywall. That’s especially unfortunate, because ACP also announced that it would invite physicians and the public to comment on this list. This is a great example of how to improve a document through crowdsourcing and leveraging the “wisdom of the crowds,” but it will only work if ACP puts the article and the survey outside of the paywall! Examples of tests that should be avoided: - Annual lipid profile for those at low risk and not on therapy - Screening tumor marker tests for ovarian cancer in those at low risk - Screening for colon and prostate cancer in those over 75 - Repeating colonoscopy in less than five years for those with benign adenomas - Doing too many tests on people who faint but have a normal neurologic exam or patients with migraine headaches - Echocardiography for those with innocent-sounding murmurs - Many preoperative tests on those at low risk - “Screening” EKGs for those at low risk Some tests that require more judgment: - If risk of heart disease is high, go directly to cardiac catheterization with angiography (more invasive.) If risk is low, instead do exercise stress tests. In all instances, do nuclear imaging with the stress test only if the patient cannot exercise or if his/her EKG is sufficiently abnormal that the EKG alone would not give a clear reading. If the risk is very, very low –don’t do any test at all! - For patients with suspected blood clots, do a sensitive blood test for those at low risk, and do an ultrasound test for those at higher risk Physicians must estimate the pre-test likelihood of a diagnosis before ordering a test. If the pre-test probability is very low, the likelihood of a false positive is often unacceptably high. If the pre-test probability of a test is very low, the likelihood of a false negative is high, and the physician should often go directly to a more invasive test. This makes it even more important to take a careful history and understand underlying risks. Physicians must be more conversant with the mathematics of test results – and the likelihood of false positives and false negatives based on pre-test probability. See a post from last year on our misguided quest for ‘certainty.’ This kind of evidence-based medicine is anything but a “cookbook.” It takes considerably more meaningful decision-making to follow these rules than to simply do an EKG on every adult. Exerting this kind of decision-making can lower the cost of health care, and can also increase the meaning of physicians’ work. An accompanying editorial in the Annals suggests these decision-making rules for physicians to consider before ordering tests (slightly condensed) · Did the patient have the test previously? (If so, is the result likely to be different and can I get the result instead of repeating the test?) · Will the test change my care of the patient? · What are the probability and consequences of a false positive? · Is there short-term danger of not ordering the test right away? · Is this primarily for patient reassurance (and if so, is there a better way to reassure the patient?) This work to identify tests often ordered unnecessarily is an excellent follow-on to the new ACP Ethics Manual, which states: Physicians have a responsibility to practice effective and efficient health care and to use health care resources responsibly. Parsimonious care that utilizes the most efficient means to effectively diagnose a condition and treat a patient respects the need to use resources wisely and to help ensure that resources are equitably available. Following these decision-making rules and eliminating these unindicated tests can help lower costs and improve the quality (and value) of health care delivery in the US. |
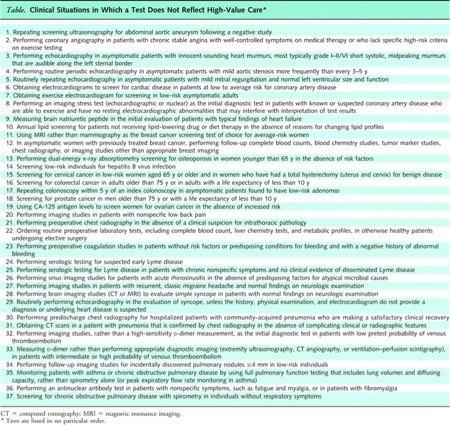
| Available at URL -but behind paywall. Click image to enlarge. |
Internists Step Up to the Plate and Identify Low Value Tests
5:10 AM
American College of Physicians, Annals of Internal Medicine, Bayes Theorem, decision-making, Tests